What's Involved with Heart Failure Diagnosis?
In most cases, heart failure develops slowly over time from long-term medical conditions, and in the early stage, may have no signs or symptoms.
Get insurance benefits, legal documents, and medical records in one place

Helpful Highlights
Despite the name “heart failure”, it doesn’t mean that the heart has actually failed or is about to stop working. It is, however, a serious and progressive condition.
In most cases, heart failure develops slowly from long-term medical conditions, though it can also start suddenly after a medical condition, event, or injury to the heart.
Sometimes a diagnosis of heart failure is a surprise and there may not have been any symptoms.
There's no one test to diagnose heart failure.
In most cases, heart failure develops slowly from long-term medical conditions. Heart failure can also start suddenly, however, after a medical condition, event, or injury to the heart muscle (such as with a heart attack). Sometimes a diagnosis of heart failure is a surprise. If your loved one has been diagnosed with heart failure, they may not have any symptoms. As the condition progresses, symptoms range from mild to severe and can be constant or come and go.
Simple physical changes that increase or do not resolve could indicate an important change in their condition. During your loved one's next visit to their primary care provider, share these subtle or ongoing changes. Most of the time, a person will tell their healthcare provider “I’m fine” because these gradual changes are now normal for them and they may not recognize those changes indicate a larger problem.
What is CHF?
Heart failure — often known as congestive heart failure (CHF), which is left-sided heart failure and the most common type — is a serious and life-limiting condition wherein the heart doesn't pump blood as well as it should.*
Despite the name “heart failure”, it doesn’t mean that the heart has actually failed or is about to stop working. It means that the heart muscle has weak contraction that limits its ability to eject blood.
This can cause blood to pool or back up in the heart, causing additional problems in the lungs and throughout the body, as well as furthering the heart's weakness.
With or without treatment, heart failure is progressive, meaning it gradually gets worse. More than 5 million people in the United States have CHF. It’s the most common diagnosis in hospitalized patients over age 65.
*While left-sided heart failure is the most common type, right-sided heart failure does occur - and on rare occasions, before left-sided heart failure (such as in cases of pulmonary hypertension, or high blood pressure in the lungs). The left side of the heart pumps blood out to the body, and the right side of the heart pumps blood to the lungs. Over time, left-sided heart failure can lead to right-sided heart failure.
Heart Failure: Quick Facts
More than 6 million U.S. adults have heart failure.
With or without treatment, heart failure is progressive, meaning it gradually gets worse.
It’s the most common diagnosis in hospitalized patients over age 65.
What can you do for your loved one?
No matter their age, accompany them to visits with their primary care provider and specialists.
Observe for subtle changes in demeanor or physical well-being and report the changes to those providers.
Ask your loved one how they feel physically and psychologically, encourage them to be honest and open with you about their experiences, and then encourage them to speak up to their providers.
Be alert for new or increased signs and symptoms, subtle changes in areas like appetite, sleep, and toileting, and indicators of depression.
Don't assume that signs and symptoms are due to existing heart failure, as there are many other possible causes, including other serious heart and lung conditions. Don't try to diagnose, call their provider.

Symptoms of CHF?
At first, there may be no symptoms or only mild symptoms. As the disease progresses, symptoms will be more bothersome.
The symptoms of heart failure depend on which side of the heart is affected (left or right) and how serious the condition has become. Most symptoms are caused by reduced blood flow to organs and fluid buildup in the body.
Shortness of breath with activity or when lying down (frequently the first noticeable symptom)
Continued fatigue or weakness, even after rest
Reduced ability to exercise
Persistent cough or wheezing
Swelling in the legs, ankles, feet, or belly (abdomen)
Difficulty sleeping while lying flat
Nausea and loss of appetite
Needing to urinate (pee) often
Rapid or irregular heartbeat
Very rapid weight gain from fluid buildup (2 lb. overnight or 5 lb. in a week)
Difficulty concentrating or decreased alertness
Chest pain, especially if heart failure was caused by a heart attack
When to see a doctor
If you think your loved one might be experiencing signs or symptoms of heart failure, make an appointment with their provider.
Call 9-1-1 if they have any of the following:
Chest pain
Severe weakness or fainting
Rapid or irregular heartbeat with shortness of breath or lightheadedness
Sudden, severe shortness of breath and coughing up white or pink, foamy mucus
Although these signs and symptoms may be due to heart failure, there are many other possible causes, including other serious heart and lung conditions. Don't try to diagnose yourself, contact a provider or emergency services.
Diagnosis
There’s no one test to diagnose heart failure. All the following are considered:
Medical history, including symptoms
Family history, including relatives who have had heart problems
Physical exam
Electrocardiogram (EKG): A painless test that reads the heart’s electrical activity, including beat pattern and any disruptions in the electrical circuit
Chest X-ray: A picture of the heart, lungs, and other chest structures that reveals whether the heart is enlarged or there are signs of lung damage
B-type natriuretic peptide (BNP) blood test: BNP is a hormone marker of the stretch or strain that the heart is under and helps determine the severity and prognosis of heart failure
Echocardiogram: An ultrasound image of the heart function. This differs from a Doppler ultrasound, which gives a picture of blood flow to the heart and lungs
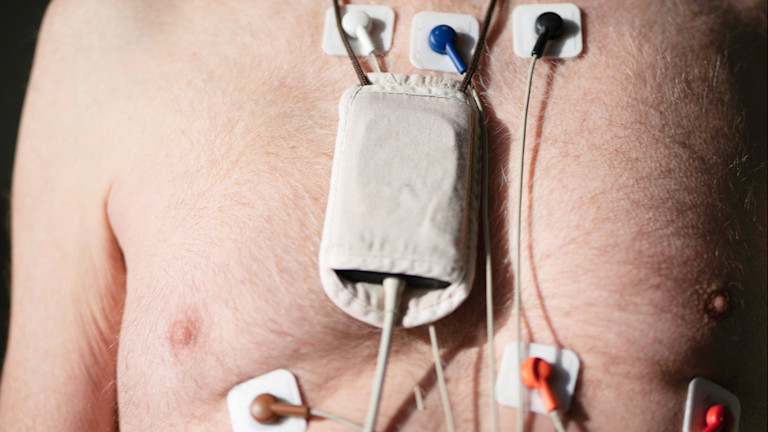
Holter monitor: A wearable device (usually 24 to 48 hours) that continuously records the heart’s electrical activity
Exercise stress test: A treadmill or stationary bicycle test to gauge how the heart performs during hard work. Some are unable to perform the exercise test, so heart stress will be induced by an injectable drug that causes a similar reaction
In some cases, the provider may make a referral to a cardiologist (a doctor who specializes in the heart) for additional tests, diagnosis, and treatment
If your loved one already has a diagnosis of heart failure and any of the symptoms suddenly become worse or a new symptom develops, it may mean that existing heart failure is no longer responding to treatment or getting worse. Promptly contact the provider.
RESOURCES
American Heart Association (AHA) – Heart Failure
American Heart Association (AHA) – Classes & Stages of Heart Failure
2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure
Caraballo, C., Desai, N.R., Mulder, H., Alhanti, B., Wilson, F.P., Fiuzat, M., et al. (2019). Clinical implications of the New York Heart Association classification. Journal of the American Heart Association, 8(23), e014240. doi: 10.1161/JAHA.119.014240
Cleveland Clinic – Heart Failure
No content in this app, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.
Get more support and guidance on insurance benefits, medical records and legal forms.
Helpful brings together your insurance benefits, legal documents, and medical records in one personalized place — so you always know what you have, and never have to search again.

Technology for Health Tasks. Mental Health for the Tough Stuff.
Helpful connects your medical records, insurance, and caregiving tasks automatically. And when you need more than logistics, a therapist is here to guide you.
In-Network and Covered
For Individuals, Couples and Families
HIPAA Compliant, Data Stays Private


Healthcare Tasks Simplified

From syncing records to spotting drug interactions, Helpful does the heavy lifting, turning complex health info into clear tasks and showing you benefits you can actually use, giving you clarity and control over your care.

In-Network Mental Health

Our licensed therapists are here to support you and your loved ones through stress, burnout, and life’s hardest moments, with an inclusive, compassionate approach that works with most insurance plans.

Create Legal Documents

Plan ahead by creating will, trusts, advance directives and more, that ensure your wishes are honored in the event you can’t speak for yourself -with Helpful guiding you every step of the way.