Urinary Incontinence Basics
Your loved one could be experiencing incontinence with no one knowing. Incontinence is the #1 reason for nursing home placement.
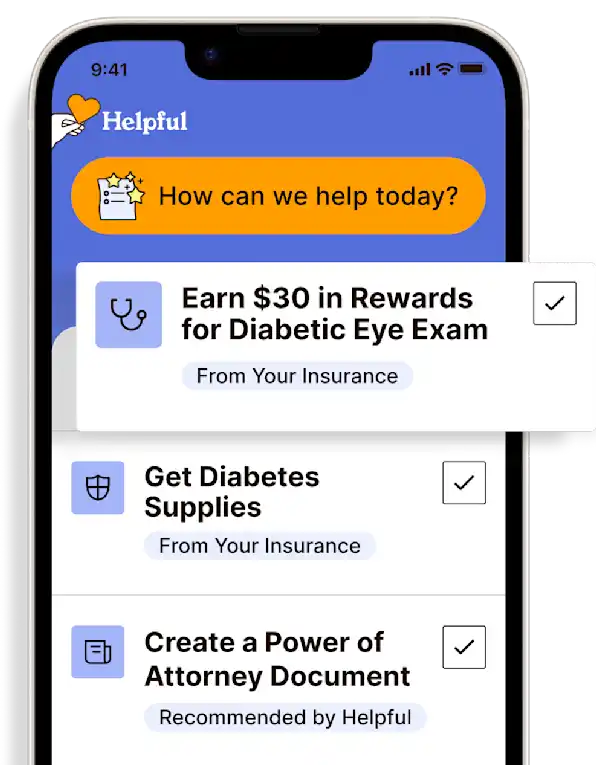
Get insurance benefits, legal documents, and medical records in one place

Helpful Highlights
Urinary incontinence is not just a "normal" part of aging.
Your loved one may be experiencing intense, negative emotions because of their incontinence.
It is important to have frank discussions with your loved one about their incontinence experience, so they maintain their dignity and independence.
There are many non-medical and medical treatments for urinary incontinence.
Urinary incontinence may affect millions of people, but it is so much more personal if your loved one is among the millions. It’s embarrassing, can interfere with daily routine, and reduce the quality of life. Managing it often becomes a concern and a complication for you, as well. It’s important to separate truth from myth regarding urinary incontinence, understand approaches and interventions, and access any available assistance from your loved one’s health plan.
Urinary Incontinence Facts
A lack of complete bladder control and a person leaks urine by accident
Over 25 million American adults have temporary or chronic urinary incontinence
It can occur at any age, though is more common in older adults, especially post-menopausal women who have had vaginal birth(s)
It is the #1 reason for placement in long-term care (nursing home)
It is the #1 contributor to urinary tract infection (UTI) in the elderly
Contrary to popular belief, even held by physicians, incontinence is not just a “normal” part of aging, especially total loss of bladder control (LINK)
4 Common Types of Urinary Incontinence
Stress incontinence occurs when activity or movement causes urine leakage or when pressure is exerted on the bladder by coughing, sneezing, or laughing. This is the most common type of incontinence and is experienced by women of all ages.
Urge incontinence occurs when there is a strong, usually sudden, urge to urinate that is difficult to delay and results in an inability to get to a toilet in time.
Overflow incontinence occurs when the urge to urinate results in only a small release of urine. The bladder gets too full and “overflows”. This can cause a constant urine leak or dribble. Men are more likely to develop overflow incontinence because of urinary retention from a bladder obstruction, enlarged prostate, or other problems.
Mixed incontinence a mixture of 2 or more types of incontinence, typically stress and urge incontinence.
There is also urinary incontinence associated with medical conditions such as severe diabetes and those that disrupt nervous system function.
Symptoms
Urine leakage that began or continued after surgery
Leaking urine during exercise or movement
Leaking urine with coughing, sneezing, or laughing
Inability to delay urination for any period, and/or needing to rush to the bathroom
A feeling of wetness without the sensation of urination
A feeling of inability to completely empty the bladder/a constantly full bladder
Your Loved One’s Concerns
Your loved one may be embarrassed when an "accident" happens in a public place or other social settings, such as family gatherings; therefore, they may withdraw from activities and gatherings to avoid embarrassment. Likewise, they may not invite others into their home because they're worried about the odor of urine on themselves or throughout the house. Using incontinence products may also lead to a loss of self-esteem and, when coupled with social embarrassment, can result in shame, isolation, and depression. Additionally, as incontinence is the #1 reason for institutionalization, your loved one may fear hospitalization or nursing home placement.
Your Concerns
While you may also be embarrassed by urine odor on them, in their home, or even in your home, it is likely you have different and greater concerns that center on safety. There is potential for injury if the floor is wet with urine, or them falling while rushing to the bathroom. Skin problems that result from moisture, and the risk for skin and urinary tract infections. Maybe you worry about the cost of incontinence products, the increase in laundry, and the physical (and emotional) demand of constant clean-ups after incontinence episodes, as well as the additional time involved in these tasks.
Treatments: Non-medical
Limit fluids after dinner
Evening fluid limitation may help with overnight bathroom trips and nighttime incontinence.
Do not limit fluids throughout the day – only after dinner
Ensure that there is adequate hydration throughout the day, and start liquids again in the morning
Avoid caffeinated drinks whenever possible, especially in the evening
Schedule bathroom breaks
Scheduling routine bathroom breaks may help eliminate rushing to the bathroom and better manage or eliminate unintended urine release.
Every 3-4 hours (setting a timer helps)
After each meal or snack
Before activities
Before naps
Before bed
First thing in the morning
This process is sometimes referred to as “toilet training” or “toileting schedule.”
Take diuretic medications (“water pills”) in the morning
Taking this particular medication early allows for enjoyment during the later part of the day and reduces incidences of overnight urination.
Incontinence wearables, bed pads, and containment systems*
Implementing urine containment products, such as pads for the bed and briefs to wear, can be difficult for your loved one and you.
For your loved one, it is a reminder that they have lost control over their body, and it may add to their embarrassment or take away their self-esteem because they feel the products are not discreet (i.e., it is obvious to everyone they are wearing them).
For you, this is a hard discussion to have with the person you are caring for because that person may feel disabled or that they are a burden. It can be especially difficult when there is a reversal in caretaking roles (the child is now caring for the parent).
Help them understand that incontinence is a common issue dealt with by millions of people, that products today are very comfortable and discreet, and that using products can return their independence and ability to participate in what they enjoy. Also, help them to have a very frank discussion with their provider about their incontinence experience.
*The BD PureWick urine collection system is the only one of its kind on the market. It is an external female catheter that manages overnight incontinence for better sleep, reduced risk of falls, and dryer skin.




Bedside commodes
These come in many configurations, including bariatric sizes.
Placed directly at the bedside overnight
Helps prevent some incontinence episodes caused by nighttime urgency
Prevents rushing to the bathroom
Avoid falls or injury due to poor night vision or limited mobility
Avoid wet bedding and wet skin, and having to change products during the night
To maintain your loved one's dignity, during the day, place the bedside commode out of sight in the tub/shower or nearby closet


Walking and core muscle exercises
Multiple studies have proven that walking reduces, and in some cases eliminates, all forms of incontinence.
30 minutes, at any pace, 5 days per week
Weight loss also promotes bladder control
Pelvic floor muscle training (PMFT)
Also known as “Kegel exercises” or simply “Kegels."
Strengthen the pelvic floor, which includes muscles of structures attached to the bladder and the bladder itself
Loose or weak pelvic floor muscles cause the bladder to "fall" when full, releasing urine
Yoga and/or Pilates
Strengthens the core muscles of the abdomen and pelvis, which helps with bladder control
Treatments: Medical
Appropriate medical treatment for urinary incontinence starts with your keen observation of your loved one’s urinary habits, including issues and changes, that are then reported to your loved one's provider.
An incontinence care plan should include:
Collaboration and cooperation with a provider
Your loved one’s opinions and preferences
Realistic expectations and goals
Medical and non-medical interventions
Therapies recommended by a provider may include:
Behavioral therapy / Bladder training
Pelvic muscle rehabilitation
Diet modifications
Medications
Nerve stimulation
Surgery
RESOURCES
American Urological Association
Continence Foundation of Australia
DeMaagd, G.A., & Davenport, T.C. (2012). Management of urinary incontinence. PT, 37(6), 345-361. PMID: 22876096
Kennedy, K.L., Steidle, C.P., & Letizia, T.M. (1995). Urinary incontinence: the basics. Ostomy and Wound Management, 41(7), 16-18. PMID: 7662091
No content in this app, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.
Get more support and guidance on insurance benefits, medical records and legal forms.
Helpful brings together your insurance benefits, legal documents, and medical records in one personalized place — so you always know what you have, and never have to search again.
Technology for Health Tasks. Mental Health for the Tough Stuff.
Helpful connects your medical records, insurance, and caregiving tasks automatically. And when you need more than logistics, a therapist is here to guide you.
In-Network and Covered
For Individuals, Couples and Families
HIPAA Compliant, Data Stays Private
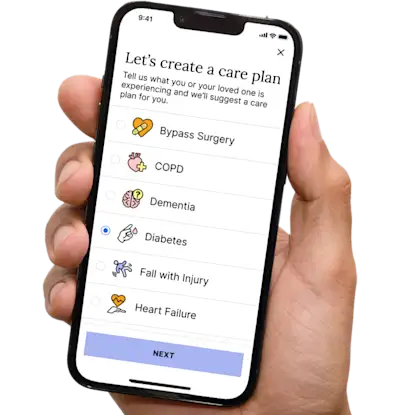

Healthcare Tasks Simplified

From syncing records to spotting drug interactions, Helpful does the heavy lifting, turning complex health info into clear tasks and showing you benefits you can actually use, giving you clarity and control over your care.

In-Network Mental Health

Our licensed therapists are here to support you and your loved ones through stress, burnout, and life’s hardest moments, with an inclusive, compassionate approach that works with most insurance plans.

Create Legal Documents

Plan ahead by creating will, trusts, advance directives and more, that ensure your wishes are honored in the event you can’t speak for yourself -with Helpful guiding you every step of the way.