Original Medicare (Parts A & B): Skilled Nursing Facility (SNF) Care
Covers short-term, Medicare-certified SNF care for those who have benefit period days remaining and a qualifying inpatient hospital stay.
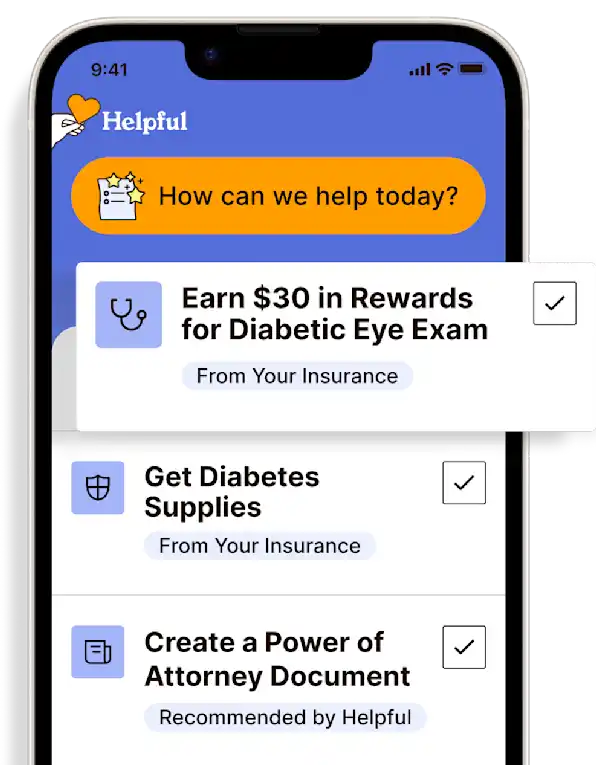
Access all my benefitsGet insurance benefits, legal documents, and medical records in one place
How To Receive
Details on how to apply
Have at least a 3-day qualifying hospital stay and obtain a provider order for admission to a Medicare-certified SNF care following hospital discharge.
Find a skilled nursing facility (SNF) near me
For more information on Medicare benefits and coverage, call 1-800-MEDICARE (1-800-633-4227) or visit the Medicare Benefits Website. TTY users, call 1-877-486-2048.
Additional Information on Costs
$0 for Days 1 - 20;
Up to $200 coinsurance each day for Days 21-100;
All costs for each day on Day 101 and beyond
Get more support and guidance on insurance benefits, medical records and legal forms.
Helpful brings together your insurance benefits, legal documents, and medical records in one personalized place — so you always know what you have, and never have to search again.
What it is
Skilled care is nursing and therapy care that can only be safely and effectively performed by, or under the supervision of, licensed professionals or technical personnel. It comprises skilled nursing and/or skilled therapy to treat, manage, and observe and evaluate care.
Medicare-covered services in a skilled nursing facility include, but aren't limited to:
A semi-private room
Meals
Skilled nursing care
Physical therapy (if needed to meet health goals)
Occupational therapy (if needed to meet health goals)
Speech-language pathology services (if needed to meet health goals)
Medical social services
Medications
Medical supplies and equipment used in the facility
Ambulance transportation (when other transportation endangers health) to the nearest supplier of needed services that aren’t available at the SNF
Dietary counseling
Things to know
While Medicare covers SNF care, there are some situations that may impact coverage and costs.
Observation services. The provider may order observation services to help decide whether admission to the hospital as an inpatient is needed or whether your loved one can be discharged. During the time they are getting observation services in the hospital, they are considered an outpatient and this time cannot be counted towards the 3-day inpatient hospital stay required for Medicare to cover an SNF stay.
Readmission to the hospital. If your loved one is in a SNF, there may be situations where they need to be readmitted to the hospital. If this happens, there's no guarantee that a bed will be available for at the same SNF if more skilled care is needed after the hospital stay. TIP: Ask the SNF if it will hold the bed in the case of readmission to the hospital. Also, ask if there's a cost to hold the bed.
Meeting the 3-day inpatient hospital stay requirement. Here are some examples of common hospital situations that show if the 3-day inpatient hospital stay requirement has been met:
Situation 1: Your loved one goes to the ER and is formally admitted to the hospital with a provider's order as an inpatient for 3 days. They were discharged on the 4th day. They DO meet the 3-day inpatient hospital stay requirement for a covered SNF stay.
Situation 2: Your loved one goes to the ER and spends one day getting observation services. Following the observation day, they are formally admitted to the hospital as an inpatient for 2 more days. They do NOT meet the 3-day inpatient hospital stay requirement for a covered SNF stay. Even though they spent 3 days in the hospital, they were considered an outpatient while getting ER and observation services. This day don’t count toward the 3-day inpatient hospital stay requirement.
Refusing care. If your loved one refuses daily skilled care or therapy, they may lose their Medicare SNF coverage. If their condition won't allow them to get skilled care (say, they get the flu), they may be able to continue to get Medicare coverage temporarily.
Stopping care or leaving. If your loved one stops getting skilled care in the SNF, or leaves the SNF altogether, the SNF coverage may be affected depending on how long the break in SNF care lasts.
If the break in skilled care lasts more than 30 days, they will need a new 3-day hospital stay to qualify for additional SNF care. The new hospital stay doesn’t need to be for the same condition that they were treated for during their previous stay.
If the break in skilled care lasts for at least 60 days in a row, this ends the current benefit period* and renews their SNF benefits. This means that the maximum coverage available would be up to 100 days of SNF benefits.
Costs
For each benefit period*, your loved one is responsible to pay:
$0 for Days 1 - 20
Up to $200 coinsurance each day for Days 21-100
All costs for each day on Day 101 and beyond
There is a 100-day limit on Part A SNF coverage in each benefit period.
*BENEFIT PERIOD: There is no limit to the number of benefit periods. A "benefit period" starts the day of admission to a hospital or skilled nursing facility. It ends after 60 days in a row without hospital or skilled nursing care. Upon hospital admission after one benefit period has ended, a new benefit period begins.
Technology for Health Tasks. Mental Health for the Tough Stuff.
Helpful connects your medical records, insurance, and caregiving tasks automatically. And when you need more than logistics, a therapist is here to guide you.
In-Network and Covered
For Individuals, Couples and Families
HIPAA Compliant, Data Stays Private
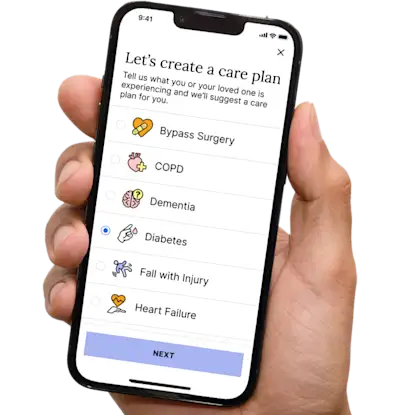

Healthcare Tasks Simplified

From syncing records to spotting drug interactions, Helpful does the heavy lifting, turning complex health info into clear tasks and showing you benefits you can actually use, giving you clarity and control over your care.

In-Network Mental Health

Our licensed therapists are here to support you and your loved ones through stress, burnout, and life’s hardest moments, with an inclusive, compassionate approach that works with most insurance plans.

Create Legal Documents

Plan ahead by creating will, trusts, advance directives and more, that ensure your wishes are honored in the event you can’t speak for yourself -with Helpful guiding you every step of the way.