Original Medicare (Parts A & B): Part A: Home Health Services
Intermittent skilled nursing, therapy, social work, and home health aide services provided in the home to support recovery or address functional decline.
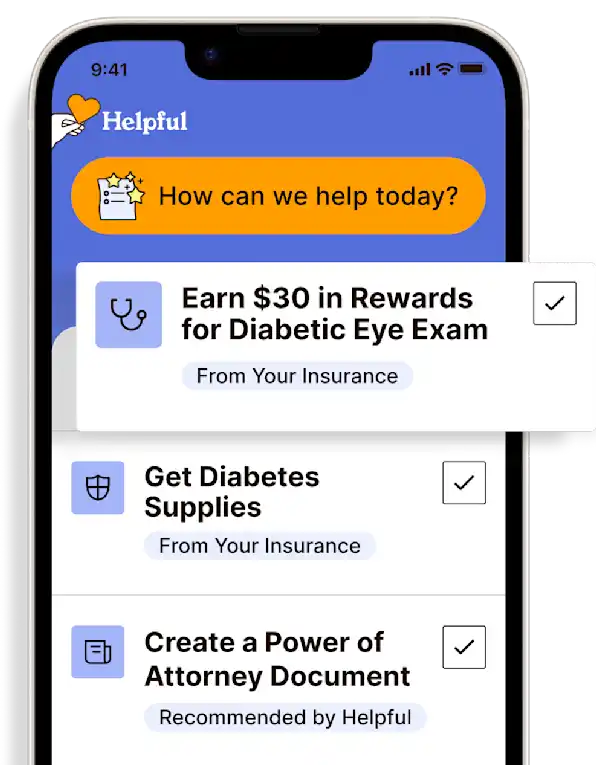
Access all my benefitsGet insurance benefits, legal documents, and medical records in one place
How To Receive
Details on how to apply
Obtain an order from a provider for home health care.
Choose a Medicare-certified home health agency from which to receive services.
Schedule an intake and start-of-care (SOC) visit.
These are typically conducted in the home by an RN, though can also be conducted by a physical therapist (PT).
Intake is generally done over the phone, though SOC is done in person and can take 2-3 hours to complete.
Together with the home health care professional, develop a plan of care and associated care goals.
The plan of care will include the services required (nursing, therapy, etc.) and a visit schedule (typically 1-3 times per week, per service).
Participate in visits, as scheduled, and complete the therapies recommended.
Home health care ends when the plan of care goals are achieved, or when there is no more progress towards goals.
For more information on Medicare benefits and coverage, call 1-800-MEDICARE (1-800-633-4227) or visit the Medicare Benefits Website. TTY users, call 1-877-486-2048.
Get more support and guidance on insurance benefits, medical records and legal forms.
Helpful brings together your insurance benefits, legal documents, and medical records in one personalized place — so you always know what you have, and never have to search again.
Medicare covers home health services under Part A and/or Part B. Medicare covers medically necessary part-time or intermittent skilled nursing care, physical therapy, speech-language pathology services, or continued occupational therapy services. Home health services may also include medical social services, part-time or intermittent home health aide services, durable medical equipment, and medical supplies for use at home.
"Part-time or intermittent" means you or your loved one may be able to get skilled nursing care and home health aide services if they are provided for less than 8 hours each day or less than 28 hours each week (or up to 35 hours a week in some limited situations).
A provider must see you or your loved one face-to-face before certifying that home health services are needed. A provider must order the care, and a Medicare-certified home health agency must provide it.
Medicare covers home health services as long as you or your loved one needs part-time or intermittent skilled services and as long as they are "homebound," which means:
They have trouble leaving their home without help (like using a cane, wheelchair, walker, or crutches; need special transportation or help from another person) because of an illness or injury.
Leaving their home isn't recommended because of their condition.
They're normally unable to leave their home because it's a major effort.
The member pays nothing for covered home health services. However, for Medicare-covered durable medical equipment (DME), they are responsible for 20% of the Medicare-approved amount and the Part B deductible applies.
Technology for Health Tasks. Mental Health for the Tough Stuff.
Helpful connects your medical records, insurance, and caregiving tasks automatically. And when you need more than logistics, a therapist is here to guide you.
In-Network and Covered
For Individuals, Couples and Families
HIPAA Compliant, Data Stays Private
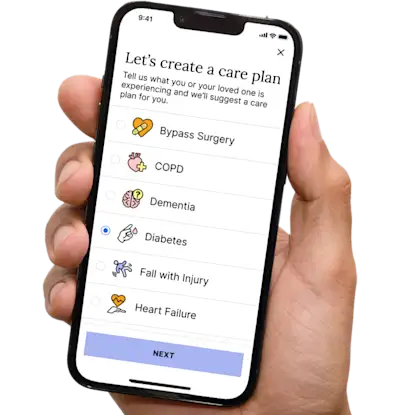

Healthcare Tasks Simplified

From syncing records to spotting drug interactions, Helpful does the heavy lifting, turning complex health info into clear tasks and showing you benefits you can actually use, giving you clarity and control over your care.

In-Network Mental Health

Our licensed therapists are here to support you and your loved ones through stress, burnout, and life’s hardest moments, with an inclusive, compassionate approach that works with most insurance plans.

Create Legal Documents

Plan ahead by creating will, trusts, advance directives and more, that ensure your wishes are honored in the event you can’t speak for yourself -with Helpful guiding you every step of the way.