Heart Attack Diagnosis and Treatment
Heart attack diagnosis is confirmed by electrocardiogram (ECG or EKG) and treatment is robust and rapid. Prepare yourself to avoid being overwhelmed.
Get insurance benefits, legal documents, and medical records in one place
Helpful Highlights
Educate yourself on all aspects of heart attack; everything from before the heart attack to years after.
There are typical (common) symptoms of heart attack, and there are atypical (unusual or unexpected) symptoms of heart attack.
Never hesitate if you even remotely suspect a heart attack, and always call an ambulance (9-1-1-) for transport.
Acute myocardial infarction (AMI), myocardial infarction (MI), ST-elevation myocardial infarction (STEMI), and non-ST elevation myocardial infarction (non-STEMI) are all terms and acronyms for heart attack.
Treatment for a heart attack includes history and symptoms, ECG (EKG), oxygen and medications, blood tests, and angiography.
What can you do?
Educate yourself regarding both typical and atypical signs and symptoms of a heart attack.
Get CPR certified (you will also learn how to operate an AED).
Learn everything you can about what happens in and to the heart before, during, and after a heart attack – the more you understand, the better you'll be able to support your loved one in the many ways they will need.
Encourage your loved one to follow provider orders. This could include medications, changes in lifestyle, cardiac rehabilitation, and the onset of depression (or anxiety).
How far in advance can people experience heart attack symptoms?
For some people, symptoms of an impending heart attack can occur for weeks or months before the actual event. For others, they experience nothing before a heart attack happens. During a heart attack, the majority of people experience typical symptoms - chest pain (pressure or squeezing) that may radiate up the left neck and jaw and/or down the left arm, heart palpitations, cold sweats, shortness of breath, and nausea. Others, especially women, and persons with diabetes, sometimes experience atypical symptoms - sudden or powerful fatigue, a general sense of unease or feeling of doom, vague chest discomfort, back pain, abdominal pain, or pain in the right shoulder area. Both typical and atypical symptoms can be experienced long before an actual heart attack occurs.
In an emergency
If your loved one, or someone around you, seems to be experiencing symptoms of a heart attack, call 9-1-1 right away. Do not ignore the symptoms and do not drive them to the emergency department yourself.
Why call an ambulance?
Emergency medical services have the equipment, medications, and personnel to start treatment for a heart attack on the way to the hospital. They can obtain an ECG (EKG) that is transmitted to an emergency physician who determines what is needed. Emergency services can make a life-and-death difference for your loved one.
Diagnosis of acute myocardial infarction (AMI, MI, or heart attack)
A physician usually diagnoses heart attacks in an emergency department setting, though as stated, they could be diagnosed "in the field" (on-site or in the ambulance).
If a heart attack diagnosis is confirmed by ECG (EKG), which means the emergency physician has diagnosed a heart attack and is beginning treatment while getting confirmation from a cardiologist, a lot starts to happen - some of which may be started in the ambulance.
History and symptoms: Personnel will ask your loved one a lot of questions about the symptoms they are experiencing, and they anyone present with your loved one to describe what happened. They will also request an up-to-date medication list and what they took today.
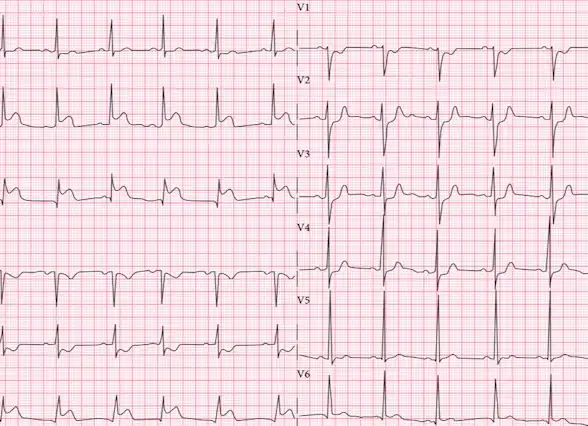
Electrocardiogram (ECG or EKG): The first test that occurs for a suspected heart attack.
Medications: Your loved one will immediately receive oxygen and 425mg of aspirin right away, usually in the form of 4 chewable tablets (81mg each), and usually a low dose of intravenous morphine (if no allergy). They may also receive a beta-blocker and nitroglycerin, on order from the physician. Ambulances have these medications available.
Blood tests: Your loved one will have many tubes of blood taken, which you'll hear referred to as "a full rainbow" because of the many different colored tops of the tubes.
During a heart attack, damage to heart muscle cells causes certain chemical markers to appear in the bloodstream. Blood tests for those markers are the most reliable methods to diagnose a heart attack and its severity.
Angiography: When a heart attack is confirmed, the hospital will prepare the cardiac catheterization lab ("cath lab") where the team will perform an intervention that allows them to look for the areas of blockage(s) in the coronary arteries.
Immediate coronary angiography for people with persistent chest pain, low blood pressure, markedly elevated cardiac markers, and unstable arrhythmias, despite treatments. The intent is to open the blockage(s) right away and restart blood flow to the affected heart muscle.
Delayed coronary angiography (within 24 to 48 hours) for people whose symptoms have resolved without complications. The intent is to detect coronary arteries and lesions (areas of damage) that may require treatment.
Angiography frequently results in a stent, in which case it becomes an angioplasty. However, if more than one major vessel is blocked, your loved one may be scheduled for bypass surgery. See content on Heart Attack: Stents vs. CABG.
Antithrombotics: Medications that break up or dissolve blood clots (blood clots are the cause of heart attacks). Administration of these medications depends on several factors and they aren't always given.
Procedures, devices, and surgery
In many cases, a minimally invasive procedure can be used to restore blood flow to the heart muscle (sometimes in combination with antithrombotics).
Balloon angioplasty and stent. During this minimally invasive procedure, a catheter (a long, thin flexible tube) is guided into the blocked artery, and a tiny balloon is inflated to clear the way so that blood flow is restored. Oftentimes, a small metal mesh cage (stent) is inserted to keep the artery open.
Atherectomy. A blade or laser is used in combination with a catheter to clear out plaque build-up in a blood vessel. You'll hear people call this "Roto-Rootering" the vessel, borrowing from the method used to clear blocked plumbing pipes.
Coronary artery bypass surgery (CABG, or simply "bypass"). A common approach used to create new routes through which blood can flow around blocked or narrowed arteries. These “bypasses” are created using healthy vessels taken from the leg, arm, or chest.
Follow-Up Treatment
Cardiac rehabilitation. Cardiac rehabilitation is a personalized 12-18 week program (36 sessions) that strengthens your loved one's heart and teaches them ways to improve heart health after a heart attack and surgery. It focuses on exercise, a heart-healthy diet, stress management, and a gradual return to usual activities. People who complete cardiac rehab are 31% less likely to have another heart attack and 47% less likely to die.
Depression or anxiety. After a heart attack, your loved one may develop anxiety or depression, or both. Nearly 25% of people do (that's 1 in 4). The medical team will work with you to help your loved one overcome these problems. See content on Heart Attack: Life After for more.
RESOURCES
American Heart Association (AHA) – Heart Attack
American College of Cardiology – Chest Pain Practice Guidelines
CDC – Heart Attack Symptoms, Risk, & Recovery
Cleveland Clinic – Heart Attack (Myocardial Infarction)
No content in this app, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.
Get more support and guidance on insurance benefits, medical records and legal forms.
Helpful brings together your insurance benefits, legal documents, and medical records in one personalized place — so you always know what you have, and never have to search again.

Technology for Health Tasks. Mental Health for the Tough Stuff.
Helpful connects your medical records, insurance, and caregiving tasks automatically. And when you need more than logistics, a therapist is here to guide you.
In-Network and Covered
For Individuals, Couples and Families
HIPAA Compliant, Data Stays Private


Healthcare Tasks Simplified

From syncing records to spotting drug interactions, Helpful does the heavy lifting, turning complex health info into clear tasks and showing you benefits you can actually use, giving you clarity and control over your care.

In-Network Mental Health

Our licensed therapists are here to support you and your loved ones through stress, burnout, and life’s hardest moments, with an inclusive, compassionate approach that works with most insurance plans.

Create Legal Documents

Plan ahead by creating will, trusts, advance directives and more, that ensure your wishes are honored in the event you can’t speak for yourself -with Helpful guiding you every step of the way.