COPD Self-Care
Your loved one wants to be independent, in control, and not a burden. They can help you by helping themselves, so guide and support them in self-care.
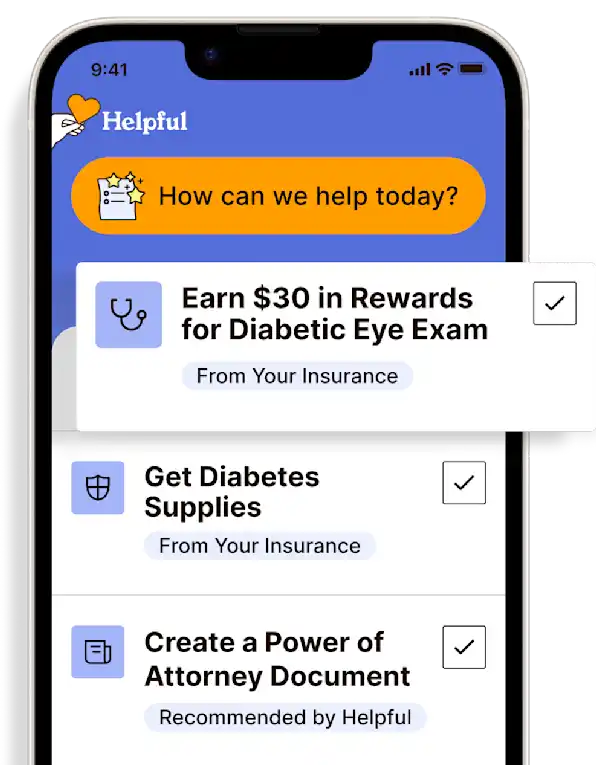
Get insurance benefits, legal documents, and medical records in one place

Helpful Highlights
Infection prevention and energy conservation are top priorities in the self-management of COPD
Other disease management strategies are more easily implemented than you may think, and you can help
COPD may have unusual symptoms that should be reported to the provider
When spending time with your loved one, incorporate encouraging conversation about self-care. Below is a list of self-care-related behaviors and tasks to help spark dialogue. Select 1 or 2 of the items that you think are most important and start there. Add more in as your loved one seems ready. These will help your loved one take the lead in their disease management and gain control over their quality of life, creating more time for you to be their loved one and not their caregiver.

Self-care (disease management)
Have a quick-relief inhaler available at all times and encourage them to use it when they feel short of breath.
Ensure they take all their medications faithfully, every day, and on time.
Get a pill box and set timers to help.
Have them eat 5-6 small meals every day rather than 2-3 big ones.
Breakfast, mid-morning, lunch, mid-afternoon, dinner, evening.
It is easier to breathe when their stomach is not full.
Advise them not to drink a lot of liquid before eating, or with their meals.
Ask a provider or a dietitian what foods boost energy and incorporate them regularly into meal planning.
If your loved one smokes, now is the time to quit.
Also, encourage them to stay away from smokers when they are out, and do not allow others to smoke in their home.
Advise them to stay away from strong odors and fumes.
Work on breathing exercises together.
This can be done with or without devices (incentive spirometer, breathing trainer)
Talk to a provider if you notice your loved one may be depressed or anxious.
Infection prevention
Having COPD makes it easier to get infections. Your loved one should get a flu shot every year and as well as ask about the pneumonia vaccine and COVID vaccine.
They should wash their hands often, and so should you.
Always wash after going to the bathroom, when returning home from being out, before preparing food, and after being around people who are sick.
Avoid crowds. Ask visitors who have colds to wear masks or to visit when they're well.
Make sure your loved one is getting plenty of vitamins and minerals that boost the immune system (examples are - but not limited to - vitamin C and zinc).
Energy conservation
Place items used most often in spots that do not require reaching or bending over to get them.
Use a cart with wheels to move things around the house and kitchen.
Use an electric can opener, dishwasher, and other things that reduce chore labor. Use cooking tools (knives, pans, dishes) that are not heavy.
Use slow, steady motions when doing things.
If available, have your loved one sit down while cooking, eating, dressing, and bathing.
Minimize going up and down the stairs.
Get help for harder tasks such as moving furniture, rearranging closets; maybe even vacuuming or taking out the trash.
Use a smaller trash can and empty it more frequently so trash bags don't get too heavy.
Advise your loved one not to try to do too much in one day.
Remind them to keep their phone with them or nearby.
After bathing, encourage them to wrap in a cloth robe or bath sheet rather than toweling off.
Look for ways to reduce stress in their life.
When to call the doctor
Call the provider if breathing is:
Getting harder
Faster than before, without a cause (such as activity)
Shallow, and cannot get a deep breath
Also, call the provider when they are:
Needing to sit and lean forward to breathe easily (known as tri-podding).
Having difficulty speaking even a few words without being short of breath.
Using chest and throat muscles to help them breathe.
The muscles and cords will stand out in the neck or the chest walls rather than the abdomen (diaphragm) moving when inhaling.
Having headaches more often.
Feel unusually sleepy or confused.
Running a temperature above or below their normal.
Coughing up dark mucus.
Experiencing bluish fingertips or the skin around the nail beds.
Experiencing bluish lips or area around the mouth.
Call 9-1-1 if they have unusual or unexplained chest pain (i.e., not from coughing).
RESOURCES
American College of Chest Physicians (ACCP) – COPD
American Lung Association (ALA) – COPD
American Thoracic Society (ATS) – COPD
COPD.com – Understanding COPD Stages & Progression
Global Allergy & Airways Patient Platform (GAAPP) – Four Stages of COPD
National Institutes of Health (NIH) Heart, Lung & Blood Institute – Lung Health Resources
No content in this app, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.
Get more support and guidance on insurance benefits, medical records and legal forms.
Helpful brings together your insurance benefits, legal documents, and medical records in one personalized place — so you always know what you have, and never have to search again.
Technology for Health Tasks. Mental Health for the Tough Stuff.
Helpful connects your medical records, insurance, and caregiving tasks automatically. And when you need more than logistics, a therapist is here to guide you.
In-Network and Covered
For Individuals, Couples and Families
HIPAA Compliant, Data Stays Private
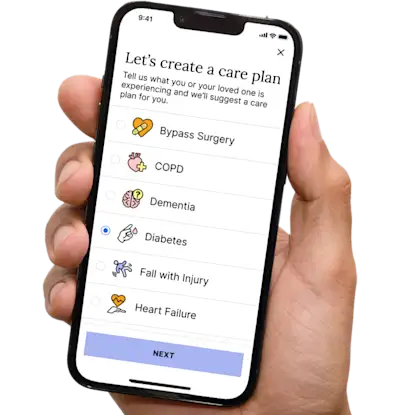

Healthcare Tasks Simplified

From syncing records to spotting drug interactions, Helpful does the heavy lifting, turning complex health info into clear tasks and showing you benefits you can actually use, giving you clarity and control over your care.

In-Network Mental Health

Our licensed therapists are here to support you and your loved ones through stress, burnout, and life’s hardest moments, with an inclusive, compassionate approach that works with most insurance plans.

Create Legal Documents

Plan ahead by creating will, trusts, advance directives and more, that ensure your wishes are honored in the event you can’t speak for yourself -with Helpful guiding you every step of the way.