VNS Health MLTC: Medical Equipment, Surgical Supplies, Respiratory Therapy, and Oxygen
Coordination with providers and vendors for required medical equipment, supplies, respiratory therapy, and oxygen.
Access all my benefitsGet insurance benefits, legal documents, and medical records in one place
How To Receive
Details on how to apply
If you have a DME/Supply order, upload it by clicking the button above
Requesting DME made easier: explore for specific guidance on Heavy DME Items (wheelchair, hospital bed, lifts, etc.), Oxygen Therapy and Wound Care.
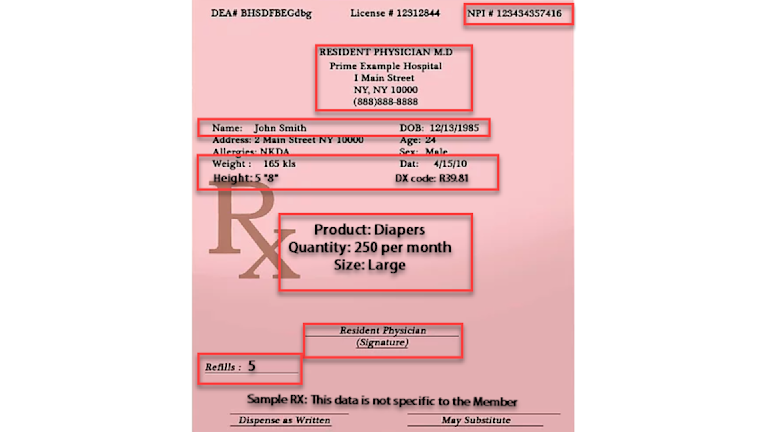
All DME Prescriptions will require at least:
Date
Member's legal name
Member's date of birth
DME-related diagnosis and associated ICD-10 codes
Provider's NPI
Requested DME/Supply product(s)
Length of need/refills
Provider signature with date
If the provider is going to send the DME/Supply order directly, then fax it to 212-897-9448
If you have taken these steps but still need assistance, the VNS Health MLTC Care Team is available to support you. Any member of the Care Team can research and respond to inquiries and questions regarding DME/Supplies. Issues will be escalated to your Care Manager if needed.
Contact the VNS Health MLTC Care Team at (888) 867-6555 (TTY 711), 9 am - 5 pm, Monday - Friday, or use the Send Us a Message form.
Get more support and guidance on insurance benefits, medical records and legal forms.
Helpful brings together your insurance benefits, legal documents, and medical records in one personalized place — so you always know what you have, and never have to search again.

Both acute and chronic conditions may require additional therapies for symptom management and treatment of the condition itself. These additional therapies may be temporary or they may be needed long-term. The Care Manager will coordinate with appropriate healthcare professionals and suppliers on required medical equipment, supplies, respiratory therapy, and oxygen.
Sometimes supplemental nutrition may be required and is part of this benefit.
In the event that supplemental oral or enteral (feeding tube) nutrition is needed, the provider will identify the mixture and route and the Care Manager will request enteral or oral supplements based on the following Medicaid Criteria:
A documented diagnostic condition where caloric and dietary nutrients cannot be absorbed or metabolized.
Clinical findings related to malnutrition.
The condition requires supplemental nutrition.
Demonstrates documented compliance with an appropriate medical and nutritional Person Centered Service Plan.
Laboratory data related to malnutrition.
A failure to increase or maintain body weight with usual solid or oral liquid intake.
Already on tube feedings.
Medicaid coverage of enteral formula and nutritional supplements is limited to individuals who cannot obtain nutrition through any other means, as well as limited to the following three conditions:
Individuals who are fed via nasogastric (NG tube), jejunostomy (J-tube), or gastrostomy tube (G-tube or PEG tube);
Individuals with rare inborn metabolic disorders;
Children up to age 21 who require liquid oral enteral nutritional formula when there is a documented diagnostic condition where caloric and dietary nutrients from food cannot be absorbed or metabolized.
Coverage of certain inherited diseases of amino acid and organic acid metabolism shall include modified solid food products that are low protein or that contain modified protein.
Technology for Health Tasks. Mental Health for the Tough Stuff.
Helpful connects your medical records, insurance, and caregiving tasks automatically. And when you need more than logistics, a therapist is here to guide you.
In-Network and Covered
For Individuals, Couples and Families
HIPAA Compliant, Data Stays Private


Healthcare Tasks Simplified

From syncing records to spotting drug interactions, Helpful does the heavy lifting, turning complex health info into clear tasks and showing you benefits you can actually use, giving you clarity and control over your care.

In-Network Mental Health

Our licensed therapists are here to support you and your loved ones through stress, burnout, and life’s hardest moments, with an inclusive, compassionate approach that works with most insurance plans.

Create Legal Documents

Plan ahead by creating will, trusts, advance directives and more, that ensure your wishes are honored in the event you can’t speak for yourself -with Helpful guiding you every step of the way.