AZ Blue Best Life Classic (HMO): Inpatient Hospital Care
Inpatient care is defined as admission into the hospital under inpatient status.
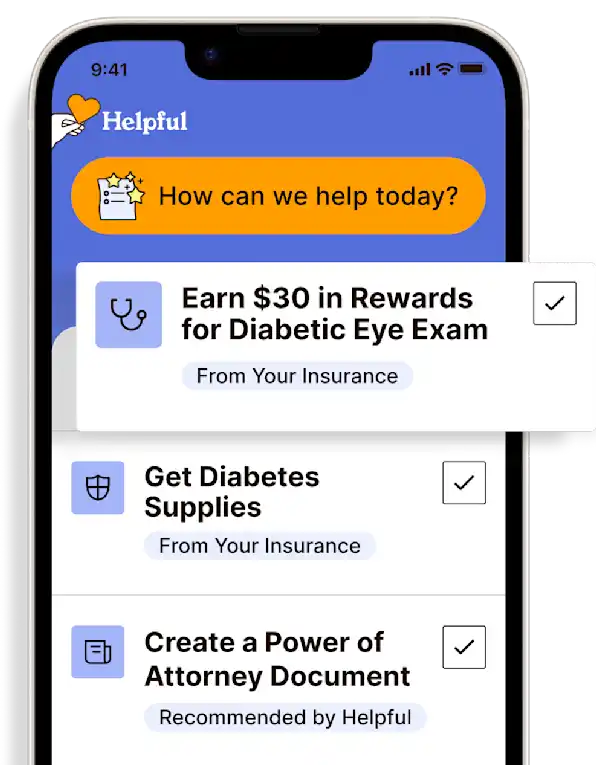
Access all my benefitsGet insurance benefits, legal documents, and medical records in one place
How To Receive
Details on how to apply
Obtain a provider order for inpatient admission.
This order will go directly to the inpatient facility (hospital, rehab, LTAC, etc.)
Except in an emergency, authorization is required for inpatient hospital care.
The admitting provider or facility may assist with prior authorization.
If inpatient care is received at an out-of-network hospital after the emergency condition is stabilized, the cost is the cost-sharing that would be paid at a network hospital.
Contact the AZ Blue Best Life Classic Team at 1-800-446-8331 (TTY 711) for authorization questions or concerns.
Work with the inpatient care team on treatment during stay and preparation for discharge planning.
Get more support and guidance on insurance benefits, medical records and legal forms.
Helpful brings together your insurance benefits, legal documents, and medical records in one personalized place — so you always know what you have, and never have to search again.
Inpatient care begins upon admission into the hospital as an inpatient (i.e., not as observation, which is still outpatient). Settings include inpatient acute, inpatient rehabilitation, long-term acute care hospitals (LTAC), and other types of inpatient hospital services. Inpatient hospital care starts on the day of formal admission into the hospital with a provider’s order and begins the benefit period (see below). The day before discharge is the last inpatient day. Except in an emergency, the provider must inform the plan of hospital admission.
Covered services include but are not limited to:
Semi-private room (or a private room if medically necessary)
Meals including special diets
Regular nursing services
Costs of special care units (such as intensive care or coronary units)
Drugs and medications
Lab tests
X-rays and other radiology services
Necessary surgical and medical supplies
Use of appliances, such as wheelchairs
Operating and recovery room costs
Physical, occupational, and speech-language therapy
Inpatient substance abuse services
Under certain conditions, some transplants are covered
Blood - including storage and administration*
Physician services
To be an inpatient, the provider must write an order for admission as an inpatient of the hospital. Even if there is an overnight stay in the hospital, it might still be considered an outpatient. If inpatient or outpatient status is unclear, ask the hospital staff.
BENEFIT PERIOD: There is no limit to the number of benefit periods. A benefit period starts on the day of admission into a hospital or skilled nursing facility. It ends after 60 days in a row without hospital or skilled nursing care. Upon hospital admission, after one benefit period has ended, a new benefit period begins.
If inpatient care is received at an out-of-network hospital following the stabilization of an emergency condition, the coverages and costs will be the same as a network hospital. Admission to an out-of-network hospital without a preceding emergency, however, will cost more. For admissions without a preceding emergency (such as direct from a provider's office or outpatient facility), the provider should choose a network hospital.
*Coverage of whole blood and packed red cells begins only with the fourth pint of blood needed—costs for the first 3 pints of blood in a calendar year must be paid out-of-pocket or the blood must be donated from self or by someone else. All other components of blood are covered beginning with the first pint.
Technology for Health Tasks. Mental Health for the Tough Stuff.
Helpful connects your medical records, insurance, and caregiving tasks automatically. And when you need more than logistics, a therapist is here to guide you.
In-Network and Covered
For Individuals, Couples and Families
HIPAA Compliant, Data Stays Private
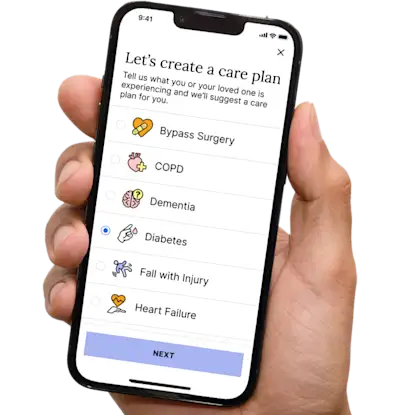

Healthcare Tasks Simplified

From syncing records to spotting drug interactions, Helpful does the heavy lifting, turning complex health info into clear tasks and showing you benefits you can actually use, giving you clarity and control over your care.

In-Network Mental Health

Our licensed therapists are here to support you and your loved ones through stress, burnout, and life’s hardest moments, with an inclusive, compassionate approach that works with most insurance plans.

Create Legal Documents

Plan ahead by creating will, trusts, advance directives and more, that ensure your wishes are honored in the event you can’t speak for yourself -with Helpful guiding you every step of the way.